March 2024 marks four years since the coronavirus outbreak and the global pandemic lockdown started. I wrote several articles spanning February – April 2020, sharing information and making some projections. This is a good time to reflect on the past and what we’ve learned and look forward to the future. Here are links to all my posts in the series with summaries of what we knew then and now. I’ll end this retrospective with my future projections. There are fifteen posts – feel free to read only the ones that jump out as you browse the titles!
Chapter 1 – What is a Coronavirus? – February 18, 2020
Then: We knew very little about SARS-COV-2, other than it was similar to about six other known viruses. Originating somewhere in continental China, the virus spread quickly, but the transmission pathways were unclear, thus the reason for the global quarantine. Washington state had some of the earliest diagnosed cases of COVID-19 in the USA. We had no rapid diagnostic tests or readily available tools to monitor its spread. Treatments and vaccines were also non-existent (although platforms for development were available – see below).
Now: We can rapidly distinguish COVID-19 from other viral infections and determine our infectivity using at-home antibody tests. Our medical system knows a great deal about disease symptoms, and we have antiviral medications that are effective for mild to moderate cases. Criteria are available to help us evaluate our risk of infection, and we understand which prevention measures work. We also have effective vaccines developed on several platforms, including mRNA platforms which were in late-stage development in March 2020. Our public health department routinely monitors wastewater systems for early detection of increases in viral diseases. The CDC and WHO maintain up-to-date databases on COVID-19 case numbers and hospital admission rates. [1,2]
Chapter 2 – Emergency Use Authorization of a Diagnostic Test for COVID-19 – February 20, 2020
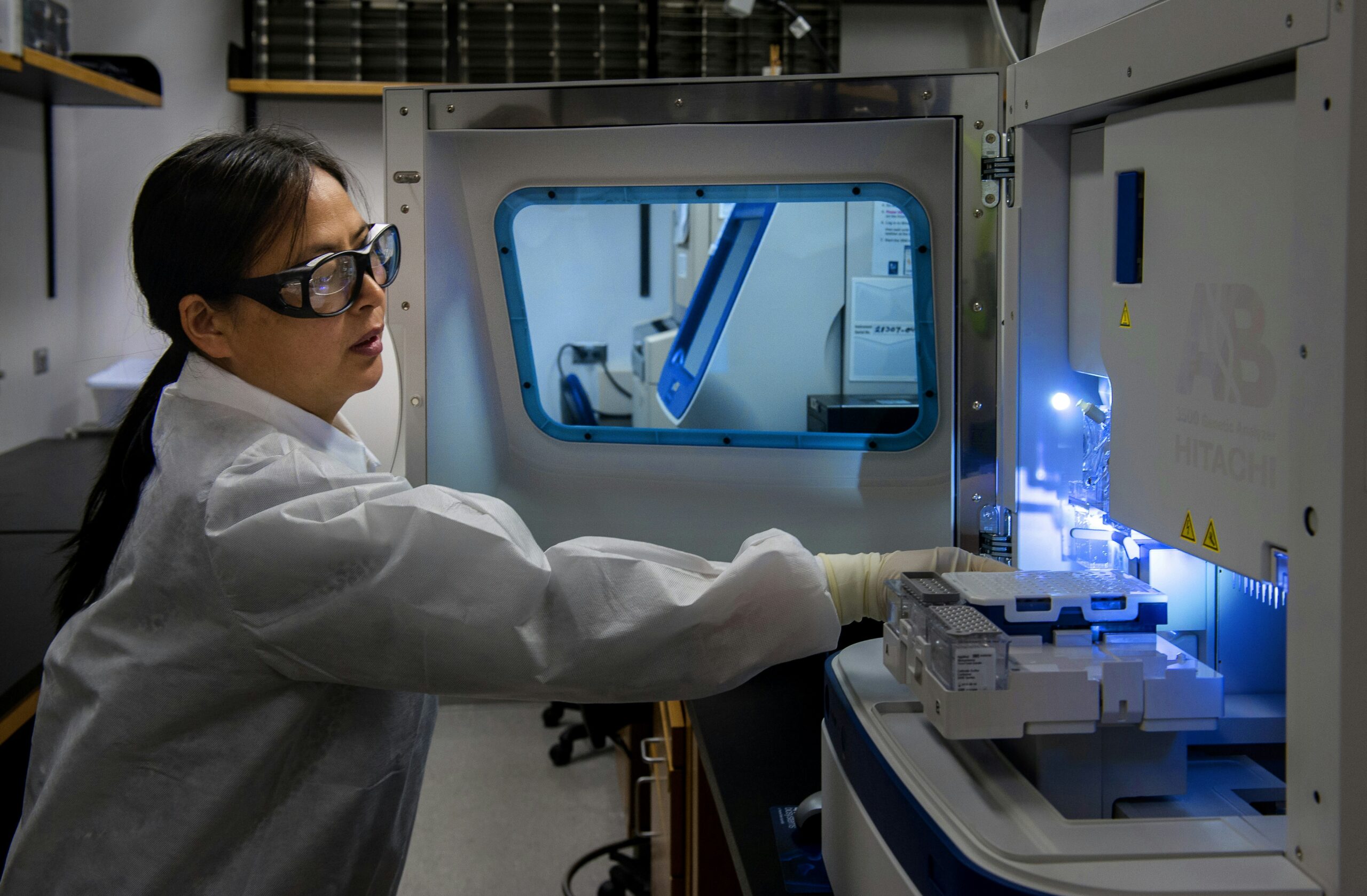
Then: One of the most urgent needs was a diagnostic test distinguishing COVID-19 from other serious respiratory viruses. One of the earliest tests was developed at the CDC. It used reverse-transcriptase polymerase chain reaction (RT-PCR) to amplify COVID-19-associated DNA fragments and produce a fluorescent signal when they were detected. The FDA used an Emergency Use Authorization (EUA) to permit commercial production and use of this test. Only labs designated by the CDC as qualified could receive test materials and perform the assay.
Now: We have multiple test options using molecular diagnostic and antigen detection strategies. The FDA further developed the EUA framework during and after the public health emergency to “help strengthen the nation’s public health protections against chemical, biological, radiological, and nuclear (CBRN) threats, including infectious diseases.” [3] The EUA was used for COVID-19 vaccines and therapies and additional diagnostics.
Chapter 3 – Controlling the Spread of COVID-19 – Global Response – February 25, 2020
Then: The risk of infection in the US was considered low. Because there were no known vaccines or treatments, public health experts recommended risk assessment and management combined with travel restrictions to and from affected areas to control the spread. I shared a webpage in the article with the CDC’s risk assessment and management advice that is now outdated and no longer available. We were approximately four weeks away from the start of the global lockdown.
Now: The CDC continues issuing new risk assessment and management recommendations as seasonal Respiratory Virus updates. [4] New variants of SARS-COV-2 arise regularly, but most pose no additional risk to the general population. As of the beginning of 2024, the JN.1 variant was the most common, and the available vaccines, tests, and treatments work against this variant.
Chapter 4 – Controlling the Spread of COVID-19 – Our Actions Help – February 27, 2020
Then: What we knew about the virus was changing daily, but it was clear COVID-19 was primarily a respiratory disease. Public health agencies re-emphasized the essentials of prevention. Years of data prove that handwashing for at least 20 seconds is the most effective means to prevent transmitting infections. [5] Other well-established recommendations include staying home when sick and covering your mouth and nose when sneezing or coughing.
Now: Nevertheless, we aren’t good at remembering to wash our hands. A CDC team led by Dr. Julia Haston surveyed U.S. adults on their handwashing behavior in June 2020 and compared rates to data from October 2019. They asked participants to self-report whether they remembered to wash after six everyday situations. They found that “despite improvements, <75% of survey respondents reported remembering to wash their hands in these situations in 2020.” [6] If the only behavioral change we apply consistently is handwashing, it would be a huge win for control of all types of transmissible disease.
Chapter 5 – Stay Up-To-Date Using Public Health Web Sites – March 3, 2020
Then: We were hungry for information by early March as infection rates increased and news reports became increasingly frantic. We were also subjected to a range of misinformation through various feeds. I shared two reliable sources online – the CDC’s COVID-19-dedicated page and the WHO’s daily situational reports. Infectious disease experts at both organizations were acquiring and evaluating the latest data on the outbreak and providing actionable summaries and recommendations through these sites.
Now: Both sites remain the best sources for reliable data summaries and the latest recommendations on protecting yourself and your family from SARS-COV-2 infection. [7,8] The WHO has some of the most interesting and effective infographics on COVID-19, including their dashboard. [9]
Chapter 6 – Biomedical Mobilization Against COVID-19 – March 24, 2020
Then: There was no better time in human history to mobilize a response to COVID-19 in the drug and vaccine development community. I watched a JP Morgan webcast on March 20th that listed 64 treatments or vaccines under active development. Some proposed treatments were already approved for other indications, with the new indication based on in vitro testing against virus samples. The WHO initiated a global clinical trial for the most promising of the existing medicines. mRNA vaccines were being tested for other infectious diseases, and companies quickly started pivoting these platforms toward SARS-COV-2. This work was helped by international collaboration among researchers, who shared the viral gene sequence within hours of confirmation, and among companies, who collaborated to decrease development timelines. Public health authorities worked together to share best practices with health care practitioners (with varying levels of success and not without some drama).
Now: We know much more about the virus and its associated conditions. Much of the early information about proposed treatments wasn’t replicable in the clinic. We learned much about how pivotal clinical trials work and what they can demonstrate from the early vaccine safety and efficacy data. Disease spread and severity decrease with the use of vaccines and treatments. The global death rate from the disease is ~1%; however, this still represents over 7 million deaths and a much larger economic, social, and emotional impact. Roopa Naik and colleagues published a comprehensive review in October 2023 to provide medical practitioners with current information on the science, clinical treatment, and prevention of COVID-19. [10] In it, they note that while we have made significant progress, the disease continues to spread and evolve. There remains an imbalance in the global availability of vaccines and treatments which confounds a sustained response.
Chapter 7a – What to Do When There are Not Enough Lab Tests/Test Sites – March 26, 2020
Then: RT-PCR was, at first, the only way to confirm a COVID-19 diagnosis. This is a complex lab test, requiring specialized equipment, reagents, protocols, and trained personnel to perform accurately and reproducibly. Sorting out the supply and training issues to expand testing using the CDC protocol proved challenging, and the FDA responded by issuing guidance for laboratories to develop, validate, and use their own RT-PCR tests to increase diagnostic capacity.
Now: RT-PCR is still the gold standard for diagnosis; however, antigen tests with high specificity and lower sensitivity are available for point-of-care testing. These antigen tests have a high false positive rate in certain situations (such as when the test performer fails to follow the instructions). Antibody and serologic tests are available but best used for confirmation testing where appropriate. [10]
Chapter 7b – R&D for COVID-19 – Treatments and Vaccines Are in Development – March 5, 2020
Then: The only treatment for COVID-19 was the respiratory standard of care. Companies with antiviral treatments under development are assessing for activity against COVID-19 and ramping up development. Gilead’s remdesivir is one such treatment that was successfully used on the first patient in Washington state under compassionate care authority. Sanofi and Johnson & Johnson mobilized vaccine development teams with the help of the Biomedical Advanced Research and Development Authority (BARDA). The first vaccines were thought to be a year away from distribution.
Now: There are four FDA-approved treatment options for COVID-19. Additional antivirals and immune-modulating drugs are available for use under EUA. [11] Six vaccines are available, two with formal FDA approval and four with Emergency Use Authorization. [12] Extensive safety and efficacy data is available for all the vaccines, with patient record numbers in the tens of thousands. This is much more than submitted for a typical New Drug Application (NDA). These vaccines offer meaningful protection, especially when combined with defensive measures like robust handwashing and staying home when sick.
Timeline note: The scope and scale of the pandemic became clearer during the first three weeks of March. On March 11, the WHO declared a global pandemic. The U.S. declared a national emergency on March 13. The CDC maintains an excellent timeline in its online museum. [13]
Chapter 8 – More Immediate Actions by the FDA to Increase Medical Supplies – March 31, 2020
Then: The end of March is when the public first learned about medical supply shortages; hospitals had already been experiencing this issue for several weeks. The FDA issued policy and guidance to facilitate supply availability. One of these actions was expanding the availability and capability of remote monitoring devices. One significant development was the increasing use of telemedicine in the U.S. after many of its barriers were removed by Congress in early March. [14] I missed this development then, but its impact will be long-lasting.
Now: Supply chain has become an overused term, covering everything from baby formula to consumer goods. The problem persists in health care, biomedical research, and manufacturing. We’ve seen multiple product recalls associated with poorly controlled changes in raw material supplies. Development and supply of drug substances and drug products are delayed and sometimes derailed by a lack of single-use manufacturing consumables and primary packaging components. Governments are investing to increase manufacturing capabilities closer to point of use, and only time will reveal the final impact. Telehealth continues to evolve and presents a significant opportunity for innovation to address health inequity and lack of access. Dr. Shaver’s article (cited above) is an excellent summary of the progress we’ve made in this area.
Chapter 9 – Preparing for an Epidemic – April 2, 2020
Then: This post was about epidemic preparedness, something which, apart from relatively small and disconnected efforts, our communities had virtually ignored. I shared a 2015 TED talk by Bill Gates, someone who received a lot of positive and negative press during and after the months of lockdown. He shared scientifically supported and achievable ideas to develop preparedness. I also mentioned the U.S. Medical Reserve Corps as an example of existing response organizations. (Side note: I remember those civil defense barrels which Bill showed in his talk from my elementary school.)
Now: Multiple people across our communities have worked hard, sometimes heroically, in the COVID-19 response. Once again, we relied heavily on our healthcare providers and systems to the breaking point. We collaborated globally but often fought and delivered mixed messages. Bill gave a second TED Talk in 2022 on the systems we need to stop future outbreaks from becoming pandemics. [15] The assembly of people, systems, and tools he suggests will seem expensive, but the ROI can easily be demonstrated by extrapolation from COVID-19 response data. It will also have a measurable impact on global health inequities and improve the length and quality of life worldwide.
Chapter 10 – Are Your Clinical Trials Impacted by COVID-19? – April 7, 2020
Then: Clinical trial disruption was certain during the pandemic, affecting patient recruitment, enrollment, and execution of trial protocols for every kind of treatment. The pandemic slowed the development of new innovations in every therapeutic area and quite likely tanked a few promising treatments when timelines became impossible to project. The FDA released guidance on clinical trial conduct at the end of March, 2020 to address many of these disruptions.
Now: “Considerations for the Conduct of Clinical Trials of Medical Products During Major Disruptions Due to Disasters and Public Health Emergencies” issued as final guidance in September 2023. [16] I believe the FDA has improved its capacity for guidance since the pandemic, given the increased frequency of new guidance and the speed of conversion from draft to final. For example, 48 guidance documents issued between November 17, 2023 and February 6, 2024, compared to 34 issued in a similar time frame in 2019-2020. This is a 41% increase. Clinical trial recruitment has emerged as the latest challenge for medical product development, and the decentralized or hybrid approaches to address the gaps are slow to develop.
Chapter 11 – CDER Creates a Single Site for Its COVID-19 Response Activities – April 14, 2020
Then: In their pandemic response, the FDA released a flood of new and updated information and guidance, quickly outpacing stakeholders’ ability to monitor and respond to the latest updates. To address this challenge and separate information by community, the Center for Drug Evaluation and Review (CDER) created a new website for all COVID-19 activities related to drugs. This separated that content from the FDA’s general COVID-19 website, which presented a running list of everything related to the pandemic arranged by date.
Now: Updates to both pages continue, and the FDA has developed additional content focused on Emergency Preparedness and Response. [17] Items on this page point to improvements in U.S. national emergency response systems (implementation of the National Incident Management System, for example). There’s no indication of FDA engagement at the global level on this site. That work appears at the level of the Executive branch, as evidenced by a recent State department media note. [18]
Chapter 12 – Quarantine Reading List – Leadership – April 21, 2020
Then: Challenging situations should trigger reevaluating our vision and values, which could lead to a change in strategy and tactics. I shared two of the leadership books I read during lockdown.
Now: No one took me up on my challenge to share their thoughts. Both books briefly shifted my frame of reference, but neither revealed any new truths for me.
Item 13 – NIH Foundation is Coordinating a Global Research Effort – April 28, 2020
Then: the NIH launched a public-private foundation to create an international strategy for COVID-19 research. Their first initiative, known as ACTIV, included four U.S. or E.U. government agencies and sixteen pharmaceutical companies, focused on the review of the “100 potential preventives and therapeutics” known at the time of launch. [19] ACTIV stands for Accelerating COVID-19 Therapeutic Interventions and Vaccines.
Now: The ACTIV group has expanded significantly in size. Scientists in their five working groups aim to develop rapid response platforms that can apply to future outbreaks. There are six additional programs that support NIH’s strategic plan for COVID-19 research. You can learn more about these programs, explore researcher resources, and access a list of NIH-funded studies at the COVID-19 Strategic Response website. [20]
Item 14 – FDA’s Coronavirus Treatment Acceleration Program (CTAP) – April 30, 2020
Then: Recognizing that any proposed COVID-19 therapy would require focused regulatory review and feedback to speed commercial scale, the FDA created a Coronavirus Treatment Acceleration Program (CTAP). [21]
Now: One year into the pandemic, Giuseppe Novelli and colleagues reported CTAP had “more than 590 drug development programs in planning stages (i.e., antivirals, immunomodulators, cell and gene therapies, compound combinations and other active principles, vaccines excluded), more than 430 clinical trials reviewed by FDA (Food and Drug Administration) with a total of 9 COVID-19 treatments currently approved for use under Emergency Use Authorization (EUA).” [22] As of December 29, 2023, there were three approved or authorized drugs for patients with mild to moderate COVID-19 and seven drugs or therapies for patients hospitalized due to the disease. [23]
I ended the series with Chapter 14. While the lockdown and the pandemic were far from over, I had already started to fold in posts on other topics in mid-March. Both I and my audience were focusing our attention on the future and the need for medical products beyond addressing COVID-19. Furthermore, there were plenty of development processes essentially unchanged by the pandemic which I continued to explore for the benefit of my readers. In my Chapter 7a post, I predicted “there will be ample opportunity to evaluate the decisions and process flow of the current pandemic in the future.” My COVID-19 series was a personal attempt to build on my knowledge and help others make progress in a difficult time. I hope we do better in the future, and I’ll be grateful if this review sparks positive outcomes for you.
References
[1] CDC, COVID-19 website. Accessed February 2, 2024. https://www.cdc.gov/coronavirus/2019-ncov/index.html
[2] WHO, COVID-19 information website. Accessed February 2, 2024. https://www.who.int/health-topics/coronavirus#tab=tab_1
[3] USFDA, Emergency Use Authorization website. Accessed February 2, 2024. https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization
[4] CDC, Respiratory Viruses/What’s New. Accessed February 2, 2024. https://www.cdc.gov/respiratory-viruses/whats-new/index.html
[5] CDC, Handwashing in Communities: Clean Hands Save Lives website. Accessed February 6, 2024. https://www.cdc.gov/handwashing/index.html
[6] Haston JC, Miller GF, Berendes D, et al. Characteristics Associated with Adults Remembering to Wash Hands in Multiple Situations Before and During the COVID-19 Pandemic — United States, October 2019 and June 2020. MMWR Morb Mortal Wkly Rep 2020;69:1443–1449. Accessed February 6, 2024. https://www.cdc.gov/mmwr/volumes/69/wr/mm6940a2.htm
[7] CDC, COVID-19 website. Accessed February 6, 2024. https://www.cdc.gov/coronavirus/2019-ncov/index.html
[8] WHO, Coronavirus disease (COVID-19)/Situation Reports website. Accessed February 6, 2024. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
[9] WHO, WHO COVID-19 dashboard. Accessed February 6, 2024. https://data.who.int/dashboards/covid19/cases?n=c
[10] Naik R, Avula S, Palleti SK, Gummadi J, Ramachandran R, Chandramohan D, Dhillon G, Gill AS, Paiwal K, Shaik B, Balachandran M, Patel B, Gurugubelli S, Mariswamy Arun Kumar AK, Nanjundappa A, Bellamkonda M, Rathi K, Sakhamuri PL, Nassar M, Bali A. From Emergence to Endemicity: A Comprehensive Review of COVID-19. Cureus. 2023 Oct 31;15(10):e48046. doi: 10.7759/cureus.48046. PMID: 37916248; PMCID: PMC10617653. Accessed February 6, 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10617653/
[11] USFDA, “Know Your Treatment Options for COVID-19.” Accessed February 2, 2024. https://www.fda.gov/consumers/consumer-updates/know-your-treatment-options-covid-19
[12] USFDA, “COVID-19 Vaccines.” Accessed February 2, 2024. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines#authorized-vaccines
[13] CDC, CDC Museum COVID-19 Timeline. Accessed February 6, 2024. https://www.cdc.gov/museum/timeline/covid19.html
[14] Shaver J. The State of Telehealth Before and After the COVID-19 Pandemic. Prim Care. 2022 Dec;49(4):517-530. doi: 10.1016/j.pop.2022.04.002. Epub 2022 Apr 25. PMID: 36357058; PMCID: PMC9035352. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9035352/
[15] Gates, B. (2022, April). We can make COVID-19 the last pandemic [Video]. TED Conferences. https://www.ted.com/talks/bill_gates_we_can_make_covid_19_the_last_pandemic
[16] USFDA, “Considerations for the Conduct of Clinical Trials of Medical Products During Major Disruptions Due to Disasters and Public Health Emergencies.” September 2023, accessed February 6, 2024. https://www.fda.gov/media/172258/download
[17] USFDA, Emergency Preparedness and Response website. Accessed February 6, 2024. https://www.fda.gov/emergency-preparedness-and-response
[18] U.S. Department of State, United States Joins in Commitment to Strengthen Pandemic Prevention, Preparedness, and Response [Media Note]. September 25, 2023. Accessed February 6, 2024. https://www.state.gov/united-states-joins-in-commitment-to-strengthen-pandemic-prevention-preparedness-and-response/
[19] NIH, “NIH to launch public-private partnership to speed COVID-19 vaccine and treatment options [News release].” April 17, 2020. Accessed February 9, 2024. https://www.nih.gov/news-events/news-releases/nih-launch-public-private-partnership-speed-covid-19-vaccine-treatment-options
[20] NIH, NIH’s COVID-19 Response website. Accessed February 9, 2024. https://covid19.nih.gov/nih-strategic-response-covid-19
[21] USFDA, Coronavirus Treatment Acceleration Program (CTAP). Accessed February 9, 2024. https://www.fda.gov/drugs/coronavirus-covid-19-drugs/coronavirus-treatment-acceleration-program-ctap
[22] Novelli G, Biancolella M, Mehrian-Shai R, Colona VL, Brito AF, Grubaugh ND, Vasiliou V, Luzzatto L, Reichardt JKV. COVID-19 one year into the pandemic: from genetics and genomics to therapy, vaccination, and policy. Hum Genomics. 2021 May 10;15(1):27. doi: 10.1186/s40246-021-00326-3. PMID: 33966626; PMCID: PMC8107019. Accessed February 9, 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8107019/
[23] USFDA, Coronavirus (COVID-19) | Drugs website. Accessed February 9, 2024. https://www.fda.gov/drugs/emergency-preparedness-drugs/coronavirus-covid-19-drugs
